By Dr Chris Healey, JAG accreditation chair and Consultant Gastroenterologist, Airedale NHS Foundation Trust
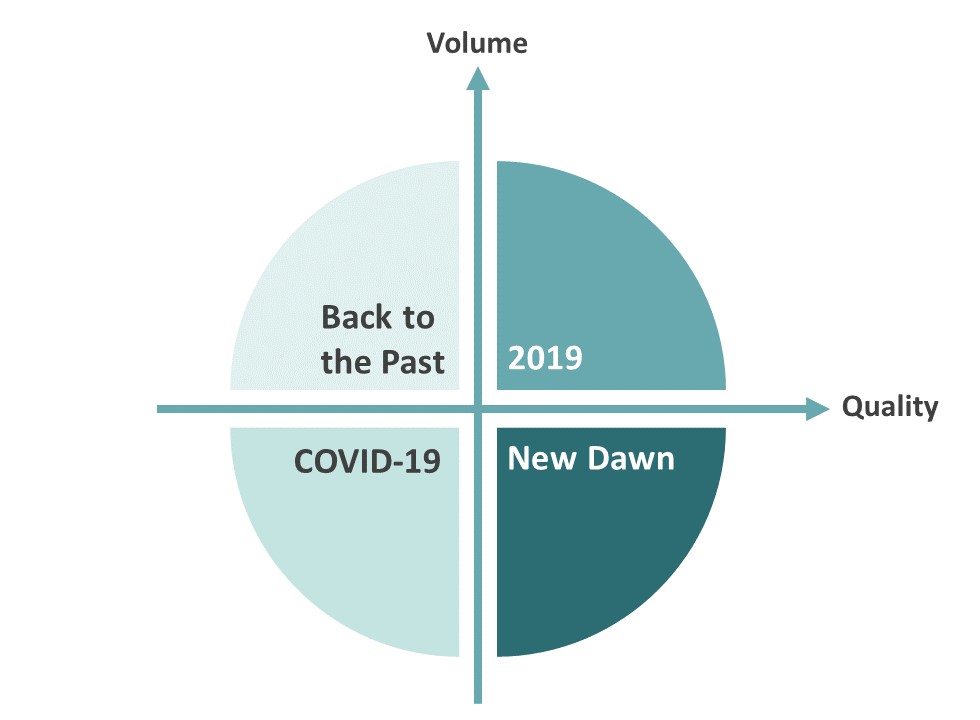
The COVID-19 pandemic has had a considerable negative effect on UK endoscopy services and has significantly reduced activity. However, it provides a unique opportunity to further improve endoscopy quality. Our recovery leads us to several potential pathways ahead. Understanding the different potential scenarios and exploring the way forward allows UK gastroenterology to maximise potential benefits and avoid any pitfalls.
‘We must choose to ‘redefine and reset’ rather than dash to hurried imperfect recovery.’
Endoscopy in 2019
The UK endoscopy landscape in 2019 was the ongoing challenge of ever-increasing demand whilst striving to improve quality. In response, endoscopy numbers have grown steadily over the last 15 years, providing rapid access to diagnosis for both fast track and routine patients. Greater public awareness of premalignant conditions, stronger clinical guidance and an aging population has led to more GI surveillance and therapeutic endoscopy (i.e. Barrett’s Oesophagus and colonic polyps).
In 2019, over 1.6 million endoscopy tests were performed by NHS England alone. The annual increase in procedures over the past five years has been >5%, with the highest growth seen in colonoscopy. Multiple initiatives were brought forward to help support endoscopy quality, helping both quality assurance and improvement. This included JAG accreditation of services and endoscopists, the JAG National Endoscopy Database (NED), the BSG endoscopy quality improvement programme (EQUIP) and the Getting it Right First Time (GIRFT) programme. The scenario of “2019” is of increasing volume and increasing quality.
The year COVID-19 hits
The COVID-19 pandemic and preparation for expected COVID-19 patients reduced both activity and quality of endoscopy. From March to April 2020, endoscopy activity reduced to 5% of previous levels with complete cessation of screening and nearly all open access upper GI endoscopy. In addition, the use of enhanced PPE and other infection control measures made the experience harder and slower for the endoscopist and more daunting for the patient. As both upper and lower tests were considered aerosol generating procedures (AGPs), without effective screening, each procedure room required additional time to let aerosol settle and to undergo thorough cleaning. Within a matter of weeks, endoscopy was launched into a new scenario of “COVID-19” where both productivity and quality decreased rapidly.
‘We now need to ask ourselves: do we go back to a world of ever-increasing demand or should we pause to reflect on our options?’
We need to avoid heading ‘Back to the Past’
We are now at a crucial point in recovery. There is considerable concern that the loss of diagnostic testing and screening will have a significant impact on cancer outcomes due to delayed diagnosis. Bowel cancer diagnoses recorded by NED are a third of previous recorded levels. This could reflect altered pathways, for example patients being diagnosed on cross-sectional imaging and going straight to surgery (omitting endoscopic and histological diagnosis). However, this is a very serious concern and is driving a desire to recover rapidly.
Indirect deaths due to COVID-19 (e.g. late stage cancer diagnosis) are a predicted outcome that needs to be mitigated. Independent sector providers have been made available to the NHS to provide surge capacity and are now providing an option of COVID-19-minimised services. In rolling out endoscopy provision to new services, there are considerable risks and pitfalls. If the desire to return to the previous volumes of endoscopy is too strong and not done with care (ie without maintaining quality), there is a real risk of a ‘Back to the Past’ scenario where poorer quality endoscopy is undertaken under eroded governance. This is the scenario of increasing volume but decreasing or unknown quality.
Looking ahead to a ‘New Dawn’
Endoscopy is a fantastic diagnostic and therapeutic tool. It is, however, invasive, carrying with it recognised morbidity and mortality. Endoscopy tests require patients to prepare and take time off (eg period of starvation and bowel cleansing) before having a sometimes frightening and uncomfortable examination. As enthusiasts for our specialism, we can easily forget or downplay such negatives.
In the light of the COVID-19 pandemic, we have been sharply reminded of the risk of our procedures and have been forced to limit endoscopy to those where there are no alternatives. When access to endoscopy and patient acceptance was growing, it was easy to order the test where doubt lay in the clinician’s mind. Such is the demand on outpatient services to see specialist consultants, where endoscopy often came first before a patient could be seen in a clinic by a clinician (ie Endoscopy 1st Consult 2nd). This has now changed and earlier clinician review should now become the operational norm. We have all been undertaking a greater review of the patient’s actual need for the test and whether there are preferable alternatives, such as FIT testing and cross-sectional imaging.
Given the previous low yield of ~3% of 2 week wait or fast track cancer pathways, such a change to ensure greater appropriateness was perhaps overdue (ie Consult 1st Endoscopy 2nd). This has real merit and is a scenario that has multiple benefits for the patient, not to mention the endoscopy services and the NHS. We have a chance to choose a ‘New Dawn’ where the quality of endoscopy continues to improve, and volume remains below that of 2019.
Our recovery scenarios
The four scenarios: 2019, Covid-19, ‘Back to the Past’ and ‘New Dawn’ are potential worlds that we can, through our recent experience, imagine and use to plan our response. If we go back to the past, concentrating on restoring volume wherever and whenever we can, the result can be foreseen of increasing missed cancers, costly repeat procedures and overall a poorer quality endoscopy product. This would not serve our patients well. We need to choose and deliver a ‘New Dawn’ where ‘less is more’, endoscopy units aiming to deliver high quality and an appropriate volume of services.
What are the characteristics of endoscopy in the UK within a new dawn?
There are many opportunities to enhance pathways, training and appropriateness within a service. Trusts and commissioners can use the momentum of review and challenge to harness the considerable enthusiasm amongst service leaders for a true reset. Finding and sharing approaches between services can lead a de facto second modernisation of endoscopy. There are great examples already: greater use of regional networking and ensuring equity across trusts; moving forward with training development and pilot regional training programme directors for endoscopy and endoscopy academies; and national implementation and clear guidance of FIT testing for diagnostic pathways. This should ensure that quality improves, and each endoscopy procedure gives better value to the patient. This fits well with a growing demand for a green revolution and a sustainable future for endoscopy.
Within JAG accreditation, we too must recognise the challenges and opportunities of recovery. The assessment process has already been reviewed and new approaches to site visits with more remote reviewing will be piloted, reducing the impact and costs to the service and assessors. A greater emphasis on clinical validation, vetting and appropriateness will be the focus of the assessment of clinical quality. Stronger infection control learnt through the experience of COVID will be reviewed and supported to enhance safety of patients and staff in a future world of multiple drug resistant organism and emerging infectious diseases.
‘2020 has been a time of disruption, but as endoscopy services recover with new norms, we must take this time to move to a ‘New Dawn’ and not ‘Back to the Past’.’