Dr Roland Valori is a consultant gastroenterologist in Gloucester and the colorectal cancer lead for NCRAS (National Cancer Registration and Analysis Service). We spoke to Dr Valori about the changes he and his team have made in vetting and surveillance in response to challenges arising from COVID-19. He discusses the unique opportunities to improve our services in a ‘new dawn’ of endoscopic practice.
COVID-19 – an opportunity for change?
Prior to cessation of all but essential endoscopy, activity had been increasing year on year.
As we recover and restart endoscopy, there is a danger that quality is sacrificed as services respond to the pressure to meet demand from deferred and new referrals.
COVID-19 has inadvertently provided us with a vehicle for change. We have the unique opportunity to readjust our focus to improve quality whilst reducing demand, filtering out unnecessary procedures and streamlining our services. This ‘new dawn’ for endoscopy is one where we can adapt and develop processes in a much shorter space of time, delivering care in a more efficient way and which is better for our patients.
Demand streams and vetting
When the pandemic started, we recognised very quickly that our vetting process needed to be overhauled. Inadequate vetting is a factor that can place unnecessary demand on a service and cause patients to undergo unnecessary procedures.
The first step was understanding where our demand for endoscopy comes from, in order to respond to and control it. Generally, there are four sources that we have identified: direct hospital referrals (clinics/inpatients), GP referrals, surveillance and screening. Recognising these sources of demand allowed us to develop a stricter vetting process and we now vet all procedures. Streamlined vetting reinforces the appropriateness of procedures undertaken and reduces the burden on our administration and clerical team.
One of the benefits of this new vetting process is tracking demand.
At present, most services will not know what their current demand is, largely due to inadequate IT systems and poor integration with endoscopy management systems (EMS). A key focus of our adapted vetting process is the potential for real-time tracking of demand by ‘time-stamping’ accepted referrals. Over time, we will be able to monitor demand in real-time and track this against our predicted demand and available capacity. Any deviances or discrepancies will allow us to adjust our capacity appropriately.
Refining surveillance
The primary goals of endoscopic surveillance are to prevent cancer and variceal bleeding. The processes that deliver this must be patient-centred and cost-effective. COVID-19 has impacted our ability to provide surveillance through delay and deferral. However, there are several strategies that we will employ to adapt and optimise delivery in the coming months.
We have already seen a significant reduction in the demand for lower GI procedures following the implementation of the recent post-colonoscopy surveillance guidelines. Additionally, we have also recently begun to look at further high-risk patient groups, identified from our study of factors contributing to post-colonoscopy colorectal cancer (PCCRC)
We identified four ‘high-risk’ surveillance groups: patients with hereditary cancer syndromes, inflammatory bowel disease, previous colorectal cancer or multiple previous large polyps. Retrospective review of surveillance referrals allows us to identify these high-risk patients and list them for procedures (approximately 10-15% of surveillance patients).
The remaining ‘low-risk’ patients can be further risk-defined through use of faecal immunochemical tests (FIT). FIT positive patients should be referred on for colonoscopy (thought to be 20% of low-risk patients). A 10µg/g threshold can be used to identify these patients and defer colonoscopy for those that are deemed low-risk and FIT negative.
Vetted referrals that are accepted are placed on a ‘future demand list’. A second stage validation is performed at 3 months prior to the procedure to ensure the patient remains suitable. A this point the patient is placed onto a ‘current demand list’. This enables tracking of demand across time.
Dedicated surveillance lists
We know that the quality of surveillance is variable. We are planning to identify individuals or groups of individuals who should perform specified procedures. In some cases, dedicated lists based on surveillance type will be introduced. This schema has been developed through mutual agreement with our upper GI surgeons, gastroenterologists and hepatologists. Each specific group takes ownership over a different procedural type e.g. hepatologists and variceal surveillance. At the point of vetting or validating the patient for surveillance we intend to be specific about what type of list the patient should be on, who can perform the procedure and the number of points needed. This will facilitate planning of lists and scheduling individual patients. We also anticipate it will improve the quality of surveillance.
Streamlining surveillance in this way allocates resources appropriately, reduces the number of unnecessary procedures and will likely improve quality over time.
Adapting IT systems
The changes and adaptations require a robust system to support them. Within our endoscopy management system (EMS), we had a pre-existing vetting module, but it was not being used and it was clear that it needed modification.
Working with developers, we adapted this module to include all key information needed for the vetting process. The vetting form allows review of referral letters, previous endoscopic history and FIT test results. We can state the number of points required for each procedure, define the category of procedure and choose who may be suitable to undertake it (including trainees). There are options for decision-making aids, including scoring systems to support vetting against guidelines. There is an internal messaging system that allows the person vetting to other users within the EMS for further opinion. This can be invaluable in complex cases and removes the added barriers created by email and endoscopy report attachments.
All data in this system is logged and time-stamped, giving us a clear idea of the number of referrals pending, those with decisions and those that have been vetted. This formalises the vetting process, timestamps demand and allows us to prospectively monitor decision-making.
Challenges
One of the biggest hurdles we had to face was changing the status quo. We had to move away from the old way of working to adjusting and incorporating a novel system. The process was time-consuming and we needed the support of all our staff to deliver this. This meant gaining engagement and support from the start and ensuring that everyone was able and supported to adjust to this new way of working.
From an IT perspective, we were limited in progress by the pace of the developer. Ideally, it would have been useful to have a ‘cloud-based’ system to enact amendments and test them in real-time and this may be a future direction. However, we are progressing at a far greater speed than we may have done prior to the pandemic. Not all services will have this level of integration of vetting, scheduling and reporting in their endoscopy reporting system. An IT solution to manage processes is not essential, it just helps. Those who do not have this functionality available but would like one should work with their ERS provider or their local hospital it and informatics teams.
What can your service do?
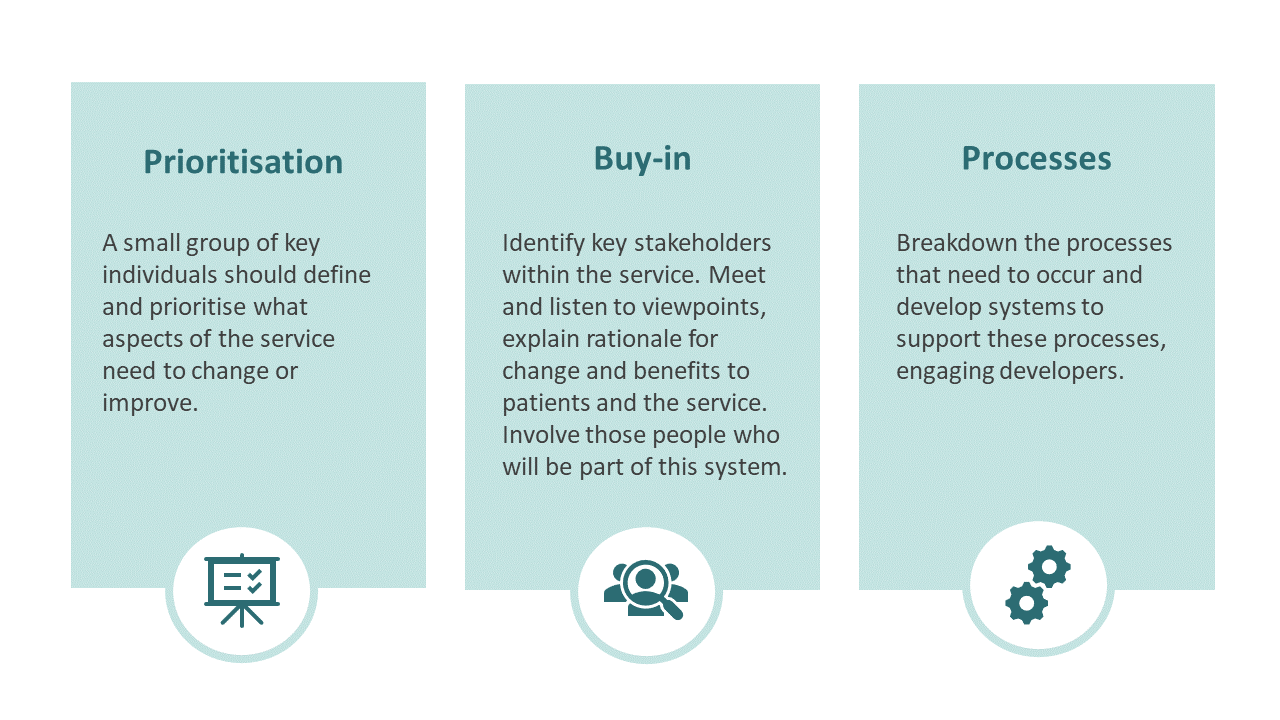
So how can services consider setting up similar changes in their units? Dr Valori highlights three key tips:
Final thoughts
We hope the system and processes we have developed will evolve to suit our needs over time. Thinking forward, we need to consider how shared decision-making and incorporating the patient voice will play a part in this process. We also need to monitor the impact of our vetting processes and surveillance lists through a variety of outcome measures.
COVID-19 has changed endoscopic practice for the foreseeable future. However, this period provides us with an unprecedented opportunity for positive change, allowing us to rejuvenate key processes within endoscopy. We should capitalise on this to drive forward the delivery of high-quality endoscopy for our patients.