Case of the month: September 2020 - safe health workers, safe patients
About this case study
This year’s World Health Organisation (WHO) Patient Safety Day was held on 17 September. In line with this year’s theme, this month’s COTM focuses on health worker safety in the wake of the COVID-19 pandemic.
Download the PDF version here and share this for discussion with your team!
Case synopsis
A morning team huddle was conducted as usual, but was incomplete as the nurse-in-charge had to attend to an unscheduled patient that had arrived in the department. As such, no equipment or personal protective equipment (PPE) issues were discussed with endoscopy team members.
Prior to the endoscopy list commencing, a team briefing was conducted with the endoscopist, the room nurses and the nurse runner (stationed outside room). No specific issues were identified until the team attended the donning station. The nurses had begun donning and the endoscopist arrived shortly after. On arrival, the endoscopist overheard a conversation between the nurses about double–checking the patient’s COVID-19 status because the PPE available to one of the nurses was not the right size. The gown did not fit and was open at the back, and the theatre hat was too small so a head covering was improvised with a plastic apron.
The endoscopist intervened to try and source the correctly-sized PPE but this was not available. A suggestion was made to attend theatres to borrow the correct PPE but this was not permitted and there were insufficient team members to swap in a different nurse. The list start time was delayed but the team recognised the importance of staff safety. The nurse in question was keen to continue with the list and did not feel the inadequately-sized PPE was a major issue. The first procedure was completed but the issue was not corrected for subsequent procedures.
This was fully discussed during a debrief at the end of the list. An action plan was escalated to the matron and the endoscopist suggested an incident report be completed but the nurse in question didn’t want to be seen to be ‘complaining’.
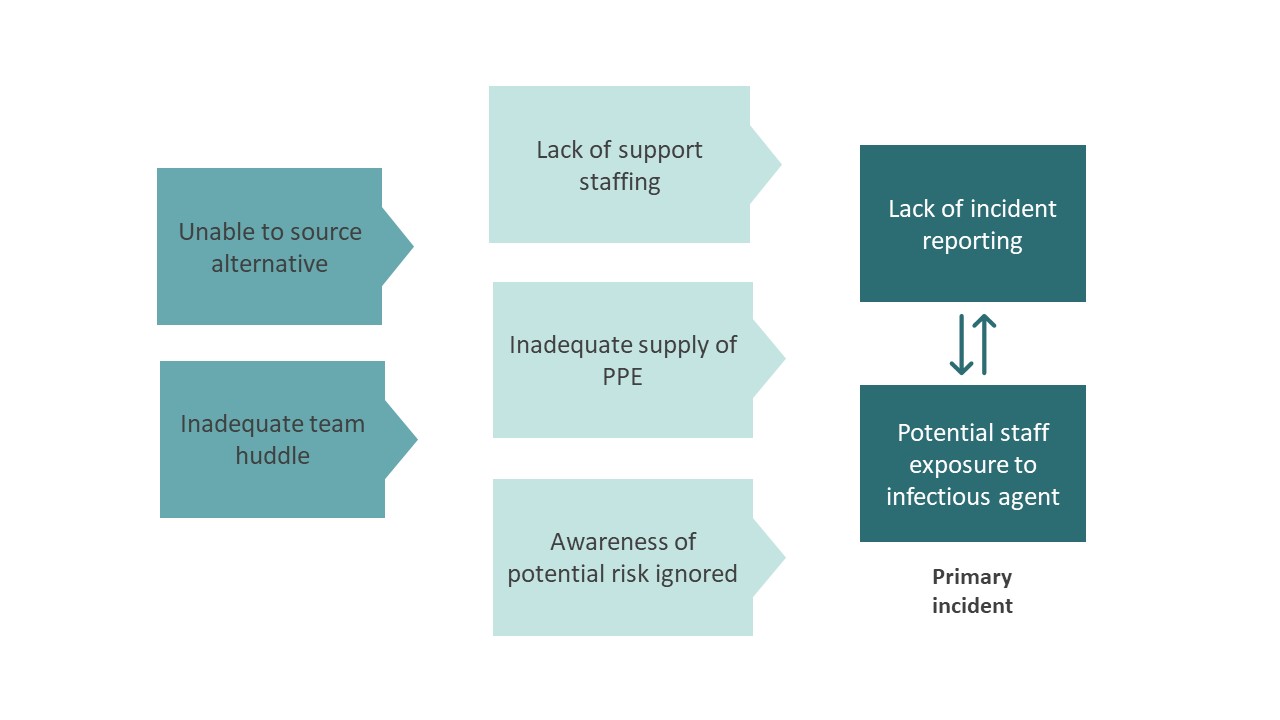
Safety incidents and contributory factors
Below is a visual representation of this case. We have highlighted the incidents involved and their contributory factors:
Learning
It is important to prioritise the safety of all staff and the provision of adequate PPE is integral to this. Similarly, staff should not knowingly expose themselves to high-risk situations. In doing so, patient safety may be consequentially affected. This responsibility lies on the team as a whole and not just the individual. A good way to remind staff about this is using the WHO slogan for this year’s patient safety day: “Safe health workers, safe patients”.
Services should ensure that PPE is available at all sites where it could be required. PPE must be available which is appropriate for different staff members, including size, gender, and race [1, 2].
Embedding a system of safety huddles, briefing and debriefing can act to ensure staff safety and wellbeing are addressed [3]. The debrief provides a safe space to discuss and resolve pertinent issues. Endoscopy team members should be encouraged to reflect on any issues in an open manner to prevent future problems.
Incident reporting should be encouraged and is a potent tool if used correctly, but we know the likelihood of reporting varies within endoscopy [4]. Reporting should be seen as an open process for learning rather than attributing blame or seen to be ‘complaining’. However, this is often difficult to embed into practice. Strong leadership and a robust bilateral feedback mechanism for the workforce may help to promote engagement [5].
References
1. TUC. Personal protective equipment and women: Guidance for workplace representatives on ensuring it is a safe fit. 2017; Available from: https://www.tuc.org.uk/sites/default/files/PPEandwomenguidance.pdf.
2. Topping, A., Sexism on the Covid-19 frontline: 'PPE is made for a 6ft 3in rugby player', in The Guardian. 2020.
3. Ravindran, S., et al., Teamworking in endoscopy: a human factors toolkit for the COVID-19 era. Endoscopy, 2020.
4. Ravindran, S., et al., Improving safety and reducing error in endoscopy (ISREE): a survey of UK services. Frontline Gastroenterology, 2020: p. flgastro-2020-101561.
5. Macrae, C., The problem with incident reporting. BMJ Quality & Safety, 2016. 25(2): p. 71.