Case of the month: November 2020 - ‘upper GI-only’ for rectal bleeding
About this case study
Download the PDF version here and share this for discussion with your team!
Case synopsis
An elderly patient with Alzheimer’s disease had an outpatient flexible sigmoidoscopy requested to assess for rectal bleeding. A consent form 4 (completed for patients lacking capacity) was completed by the referring clinician following discussion with his next of kin.
It was decided that the patient should be admitted to hospital for the procedure. A separate, inpatient referral form was completed, as per the department’s policy. During the booking process, the patient was incorrectly listed for an OGD and placed as the last patient on an ‘upper GI-only’ endoscopy list.
The patient was clerked in by a junior doctor the evening before his procedure and prepped for an OGD. The clinic letter and original referral were not reviewed. On the morning of his procedure the patient arrived from the ward without an escort as the ward was understaffed. Endoscopy had received a brief telephone handover from a ward nurse (covering for their colleague, who was on a break) who confirmed the patient had been fasted. However, they were unsure why the patient was undergoing a procedure.
The patient was brought into the room. The endoscopy team performed a checklist together but did not review the original referral in the notes or the indication on the consent form. The patient underwent an uncomplicated OGD. In recovery, the original referral was identified in the notes and, on further review, the recovery nurse identified that the procedure undertaken and that listed on consent form were different.
The endoscopist, ward team, clinical lead and nurse lead for endoscopy were notified and an investigation undertaken. The patient’s next of kin was informed and an apology provided as soon as the incident had been identified.
Safety incidents and contributory factors
Below is a visual representation of this case. We have highlighted the incidents involved and their contributory factors:
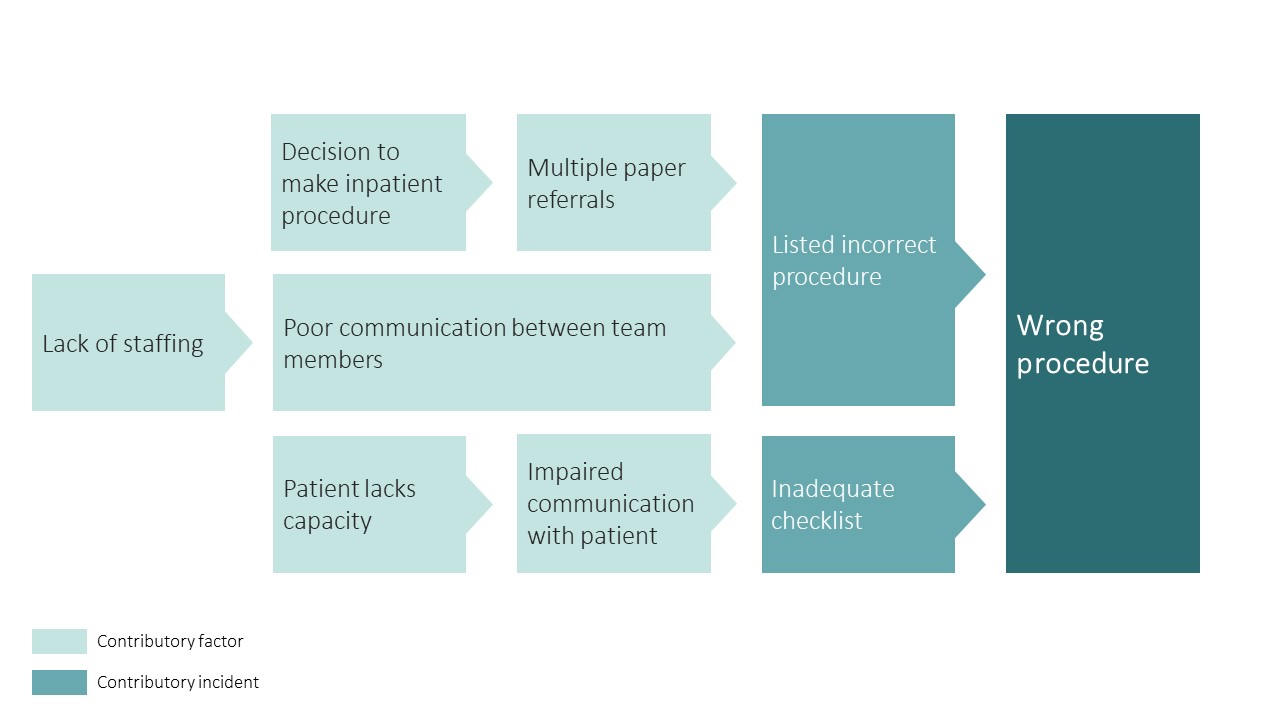
Contributory incidents and factors can be classified with a human factors approach. This is helpful in identifying areas to focus on in preventing future incidents:
| Category | Contributory incident/factor |
| Patient | Underlying cognitive impairement |
| Technology and tools | Multiple paper referrals |
| Individual (staff) | Incorrect procedure booked |
| Environment | Understaffed medical ward |
| Team | Incomplete communication between team members Lack of escort Inadequate checklist |
Learning
Never events are patient safety incidents that are wholly preventable through following pre-existent guidance and checks. Never events are not usually related to a single error but often a culmination of multiple contributory incidents and factors. Never events in endoscopy are rare but do occur; they include:
• Procedures on the wrong patient
• Procedures involving the wrong site
• Patients who undergo the wrong procedure.
Below are some important learning points felt to be relevant in this case:
1. Always complete the safety checklist ‘timeout’ by reviewing the checklist in order and ensuring indication and consent is checked prior to the procedure. This is particularly relevant where communication with a patient may be impaired (as in this case).
2. The “time-out” phase of the checklist should not be a passive process and requires engagement of ALL team members. This is the final opportunity for clarification and error detection before a procedure begins. It is easy to fall into the ‘routine’ of checklist completion, particularly during lists dedicated to a single endoscopic procedure-type. This may have contributed to the inadequacy of the checklist and ultimate error in this case.
3. Referral systems should be robust and electronic. They should allow an audit trail of the referral, highlight discrepancies and increase transparency amongst staff.
4. The admitting doctor should always complete the clerking process, ensuring that notes, clinic letters and consent forms are always reviewed. This ensures patients are prepared appropriately and identifies any potential issues prior to their procedure(s).