Case of the month: March 2021 - food glorious tubes
About this case study
Download the PDF version and share this for discussion with your team!
Case synopsis
The endoscopy team received a request from the nutrition team asking for a patient to have a PEG (percutaneous endoscopic gastrostomy) with jejunal extension. This patient had been admitted with recurrent aspiration pneumonia and already had a RIG (radiologically-inserted gastrostomy).
There was limited information on the endoscopy request form, only that the patient previously had a laryngectomy. A further discussion with the nutrition team also revealed that patient already had a surgical jejunostomy in situ, however the patient was not tolerating feed through jejunostomy as it was too far down the small bowel, causing bloating and diarrhoea.
The trust-approved PEG referral form (outlining indication, co-morbidities, physical assessment) was not completed by the referring team and was not insisted upon by the endoscopy team. The patient was being assessed by the nutrition team regularly and the request had been directly from a nutrition consultant.
The patient was brought down to the endoscopy suite and the checklist was performed with the information available. The endoscope was inserted to the back of the mouth as far as the back of the tongue. Almost immediately, it was evident there was severely altered anatomy and gauze was seen where the pharynx should be. On withdrawing the scope slowly, an area at this site started to ooze fresh blood. After withdrawal of scope 200ml of fresh blood was suctioned from the stoma in the neck.
A major haemorrhage call was initiated and the ENT team was called. The bleeding was controlled with packing and insertion of a tracheostomy tube as well as supportive measures with blood products. The patient eventually stabilised.
A debrief was held between the endoscopy and ENT team. The ENT team highlighted the patient’s history of a total pharyngolaryngectomy for pharyngeal squamous cell carcinoma. Due to complications over the years, the patient’s anatomy had been highly altered and the patient was well-known to the ENT team. They were disappointed that they had not been consulted at all during this patient’s admission.
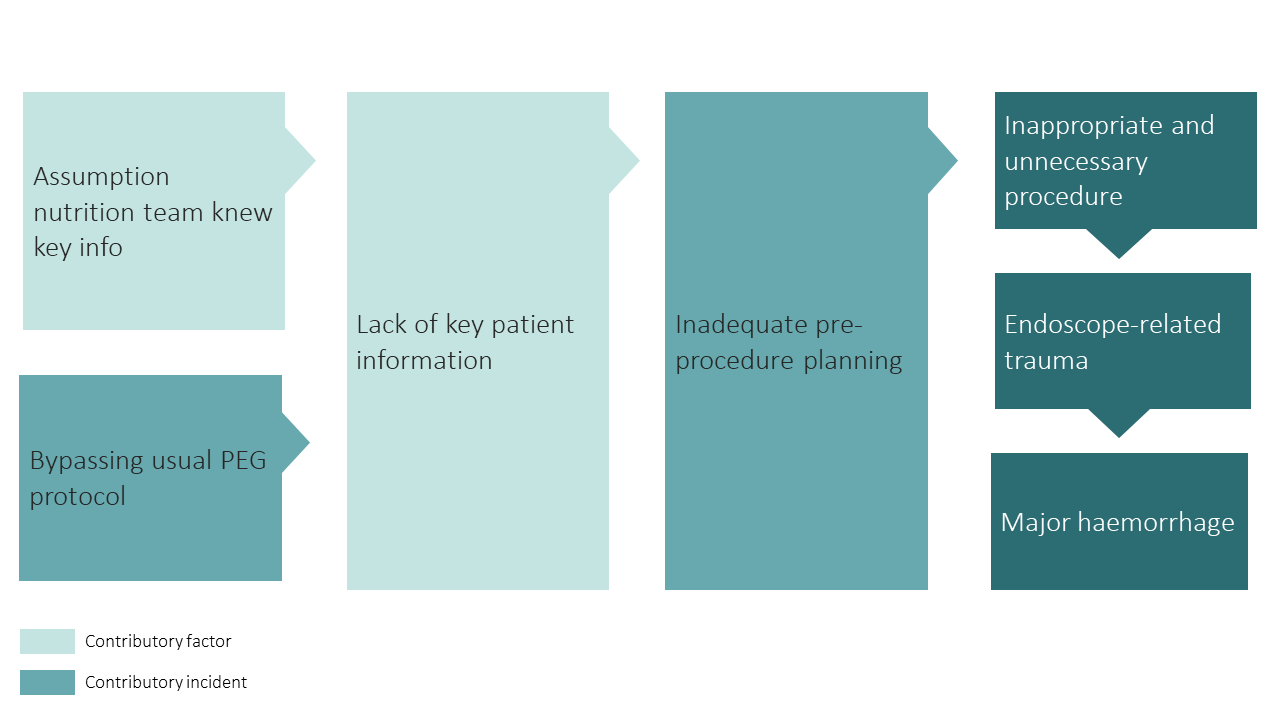
Safety incidents and contributory factors
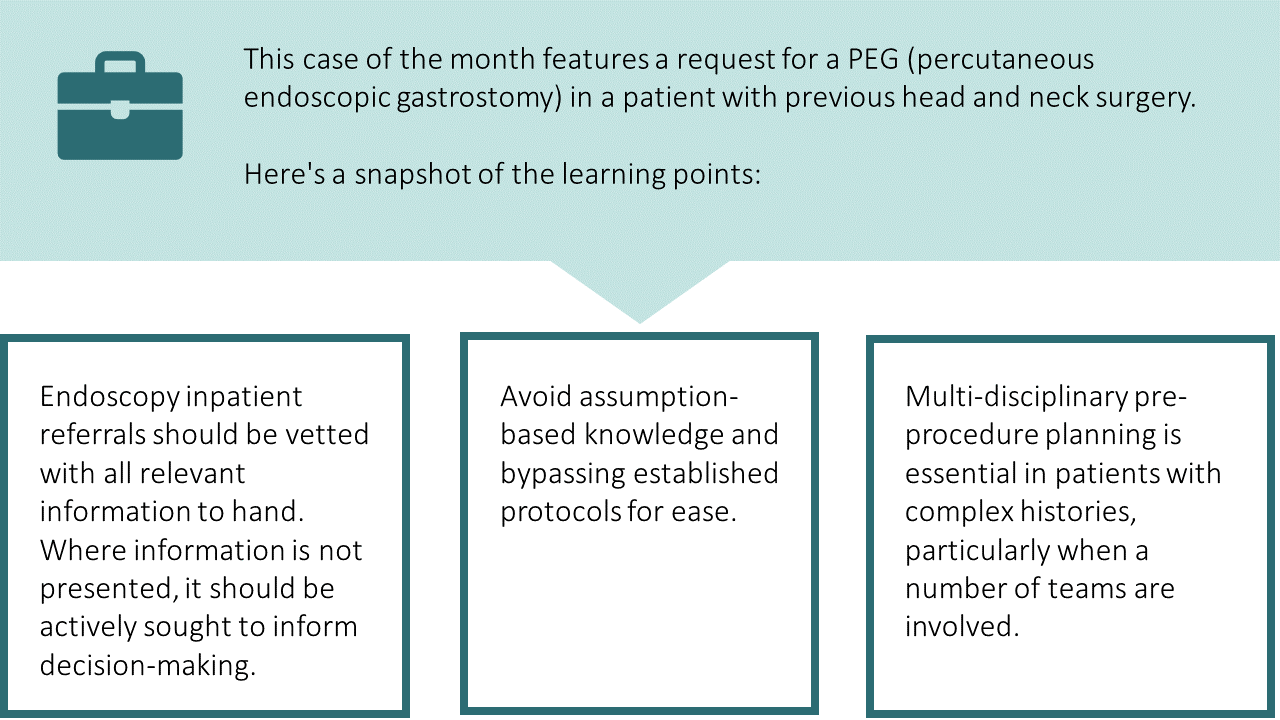
Below is a visual representation of this case. We have highlighted the incidents involved and their contributory factors:
Learning
Information gathering
1. Endoscopy inpatient referrals should be vetted with all relevant information to hand.
- Clinical decision-making in endoscopy is dependent on the quality of information provided.
- It is crucial all information is identified, especially in a complex patient such as this. This often means contacting the parent team to enquire further and attending PEG MDT discussions.
2. Referrals should include any relevant post-operative changes to anatomy.
- This is relevant in all forms of endoscopy, for example previous gastric bypass surgery in ERCP and colonic resections in lower GI endoscopy.
3. It is easy to fall into the trap of assuming information is collectively known.
- Assumptions were made that the nutrition team were aware of the patient’s full medical and surgical history.
- Additionally, trust may have been placed in the decision of the nutrition team based on their sub-specialty skills and relationship with the endoscopy team.
4. It is important that safety nets are embedded into referral systems, for example using a dedicated PEG referral form after a multidisciplinary nutrition. assessment. By not completing this, established protocols are bypassed and important information is not obtained.
- Further history revealed the patient had a previous gastrojejejunostomy performed under radiological guidance. There had subsequently been issues with the jejunal extension due to altered stomach anatomy and it was felt that a surgical jejunostomy was the only option.
- This piece of information was crucial to the decision-making process and would have meant the endoscopic procedure would not have been undertaken.
Planning
Therapeutic procedures in complex patients need specific pre-procedural planning with the referring team and the specific endoscopist under-taking the procedure.
This starts at point of referral and vetting to identify personnel, equipment, and environment for any potential procedure.
This may include involvement of other teams, which requires extra planning and coordination - in this case a briefing with the ENT team and anaesthetic team (if required).
What are your views on this case? Continue the discussion online @JAG_Endoscopy #COTM Have you had any learning points with similar experiences that you wish to share with endoscopy community? Contact askjag@rcplondon.ac.ukfor more information. |