Case of the month: April 2021 - know what's in your toolbox
About this case study
Download the PDF version and share this for discussion with your team!
Case synopsis
A patient with a history of oesophageal varices had a successful OGD for melaena, in which 3 bands were placed to stop bleeding. Unfortunately, 7 days later, the patient developed haematemesis on the ward in the early evening. The out-of-hours GI bleed consultant was called and an emergency endoscopy arranged following appropriate resuscitation. The patient was brought to the emergency theatre, anaesthetised and intubated for the procedure.
Endoscopically, there was evidence of ongoing variceal bleeding and a few unsuccessful attempts at banding were made. The endoscopist felt that further attempts at banding would not work and there was worsening haemodynamic instability due to ongoing blood loss. The endoscopist requested a Sengstaken-Blakemore tube to tamponade the bleeding. The out-of-hours endoscopy team consisted of the GI bleed consultant and theatre nurses. The nurses questioned what this piece of equipment was and where it could be found. The emergency trolley used for out-of-hours endoscopy did not seem to have this stocked. The endoscopist was unaware where they were usually kept as the endoscopy assistants/nursing staff usually manage equipment and stocks.
The procedure was abandoned and the patient transferred to ITU with supportive measures. The patient stabilised with blood products and a repeat procedure was scheduled for the morning.
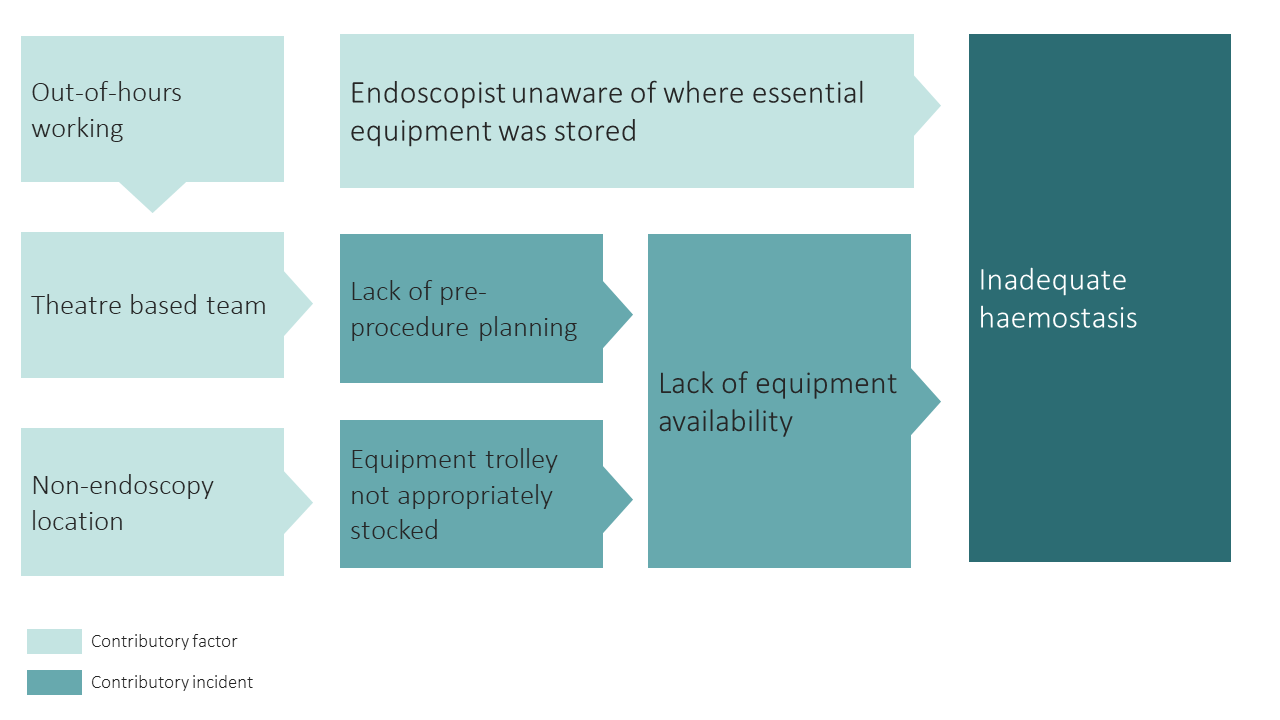
Safety incidents and contributory factors
Below is a visual representation of this case. We have highlighted the incidents involved and their contributory factors:
Learning
Out-of-hours working
- Out-of-hours working can present additional challenges above those of the ‘normal’ working day. Procedures that have to be undertaken out-of-hours are, by definition, high risk.
- Emergency out-of-hours endoscopy rotas (including GI bleed rotas) are staffed by endoscopy nurses in around two thirds of acute services.
- One challenge can be working in unfamiliar teams, for example an endoscopist working with theatre staff. It is easy to assume that all team members will be familiar with processes and equipment.
Equipment
- Emergency equipment or ‘bleed’ trolleys should be commonplace with all relevant equipment stocked necessary to undertake a procedure.
- These should be monitored and stocked appropriately. Importantly, team members should be familiar with pieces of equipment. Where new or adapted equipment is used, training should be in place to familiarise team members with its use.
- It is everyone’s responsibility to ensure the appropriate equipment for the procedure are stocked and available. This should be checked before the procedure starts.
Briefings
A pre-procedural briefing would have been useful in this case to:
- Highlight the need for specific types of equipment and their availability.
- Share potential therapeutic plan, including alternatives in order of use e.g. plan A and plan B.
- Identify any knowledge or training gaps within team e.g. purpose and deployment of Sengstaken-Blakemore tubes.
- Location of missing equipment could have been identified by other colleagues or by referring to a departmental manual.
What are your views on this case? Continue the discussion online @JAG_Endoscopy #COTM Have you had any learning points with similar experiences that you wish to share with endoscopy community? Contact askjag@rcp.ac.uk for more information. |