Case of the month: May 2021 - sweet or sour
About this case study
Download the PDF version and share this for discussion with your team!
Case synopsis
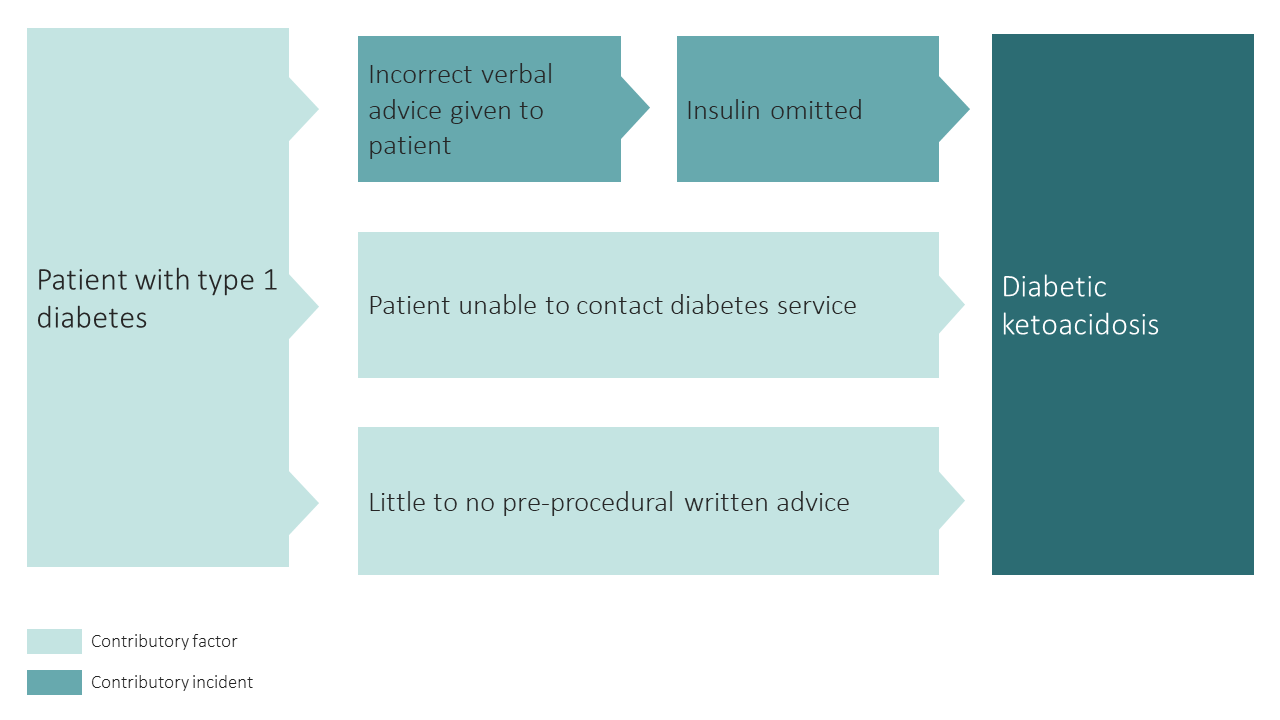
A patient with type 1 diabetes attended a colonoscopy. At admission, their blood sugar was 25 and the patient felt nauseous. The admitting nurse moved the patient to recovery for close monitoring whilst requesting a colleague to bring the blood ketone machine from a neighbouring department.
Further questioning revealed that a few days prior to their procedure, the patient had tried to get instructions from the local diabetes specialist team, but the number they were given was incorrect. The patient was taking long-acting insulin in the morning and short-acting insulin with meals (basal bolus regime). The patient then called the endoscopy department and followed instructions about insulin dosage from a healthcare professional. They were unsure who they spoke to in the department. They were told that, because they were not eating, to omit insulin from the night before the procedure. The patient therefore did not have any insulin from the evening before the colonoscopy.
On checking, the patient’s blood ketones were 6.1. The emergency medical team were contacted, and the patient was transferred to the emergency department. A diagnosis of diabetic ketoacidosis was made, and treatment promptly started.
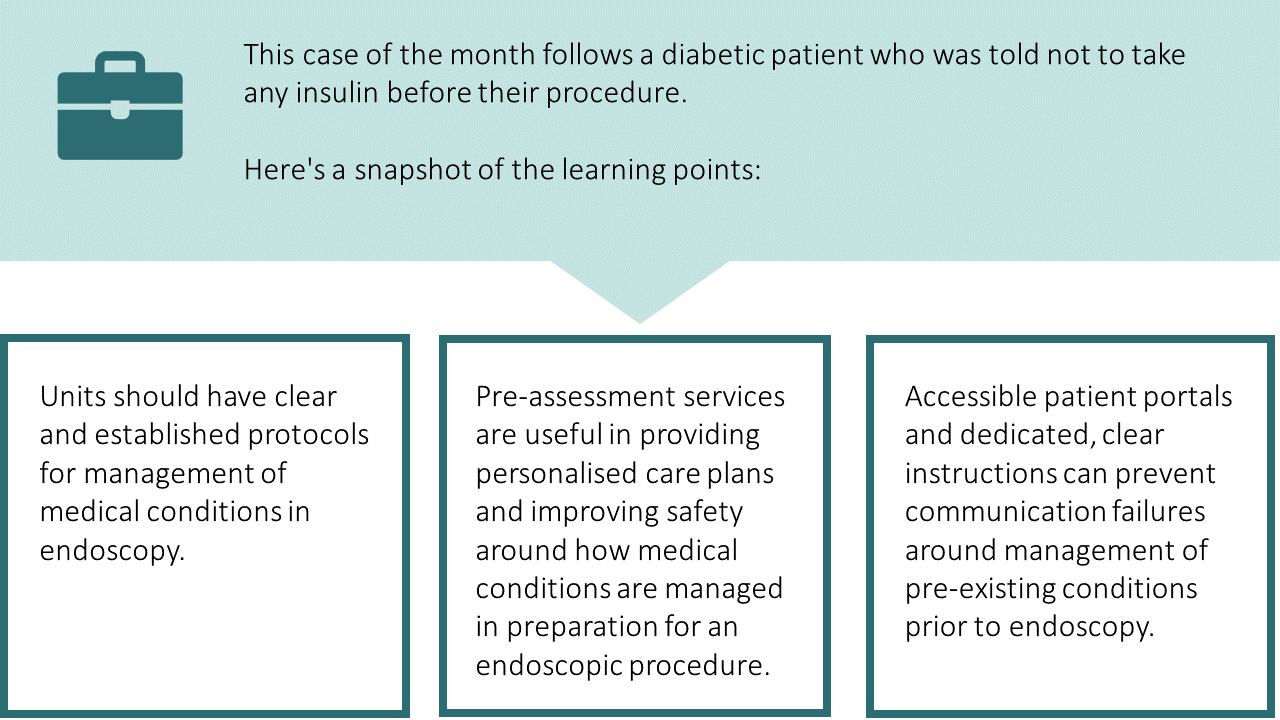
Safety incidents and contributory factors
Below is a visual representation of this case. We have highlighted the incidents involved and their contributory factors:
Learning
Diabetes and endoscopy
- Elective procedures such as endoscopy can affect usual diabetic control. This is due to factors such as fasting, bowel preparation, direct effect of procedure on blood sugar and alterations to medication.
- Incorrect management of diabetes around the time of endoscopy can lead to medical emergencies such as diabetic ketoacidosis. This has significant ramifications for the patient and a secondary impact of diverting nursing resources away from the endoscopy service and patient flow.
- Management of insulin around endoscopy is based around the type and timing of insulin doses as well as the type of procedure undertaken. Blanket advice based on nil-by-mouth status is outdated and incorrect.
- Endoscopy services should have clear policies and pathways around the management of diabetes as well as other medical conditions. This should reflect national guidance where relevant and a training programme for endoscopy team education should be in place.
Pre-assessment
- Pre-assessment services (including telephone and face-to-face) may help to improve understanding of a patient’s medical history, provide individualised care plans and give patients clear written and verbal instructions around management of pre-existing conditions.
- Some conditions such as type I DM should be prioritised for pre-assessment.
- If complex medical conditions are highlighted, other specialist teams may need to be involved to provide a carefully co-ordinated peri-endoscopy management plan.
- Pre-assessment services can improve patient safety and improve other factors related to quality such as reducing ‘Did Not Attend’ (DNA) and cancellation rates.
Communication failures
This case highlights how proper communication of instructions around medication to patients is vital. This can be achieved in numerous ways:
- Dedicated pre-assessment consultations
- Patient-friendly leaflets with clear instructions
- Accessible contact portals with up-to-date information for patient queries
- Easily accessible information for staff who respond to patient queries eg easy access to patient plan.
What are your views on this case? Continue the discussion online @JAG_Endoscopy #COTM Have you had any learning points with similar experiences that you wish to share with endoscopy community? Contact askjag@rcp.ac.uk for more information. |